In an October 2024 blog post, I explored how research on the human brain sheds light on the brain’s neurophysiology and helps clinicians devise novel treatment options for tackling treatment-resistant depression (TRD). I also highlighted specific research on how the SAINT® neuromodulation system has proven effective in treating TRD. Here, I will focus specifically on notable findings from multiple studies regarding the neuroimaging changes noticed from using SAINT therapy.
To understand fully the key implications of these studies, an explanation of several key terms is necessary. Individuals suffering from TRD do not experience relief from their symptoms from taking antidepressants and/or undergoing psychological counseling. Major depressive disorder (MDD) is a mental health condition characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in activities. It can significantly impact an individual’s daily functioning, relationships, and overall quality of life. MDD may be caused by a combination of genetic, biological, environmental, and psychological factors.”[1]
Several areas of the brain are thought to have an impact on or be impacted by depression. The prefrontal cortex (PFC), left dorsolateral prefrontal cortex (left DLPFC), and anterior cingulate cortex (ACC) all play an important role in higher-level executive functions, including the regulation of emotions, impulse control, decision-making, and memory. The amygdala—a small, almond-shaped part of the brain located in the medial temporal lobe—plays a key role in processing emotions, memory, and learning. Several techniques exist to image the brain. Of relevance here is the resting-state fMRI (rs-fMRI), which is a brain imaging technique that measures spontaneous fluctuations in brain activity while a person is at rest.
In 2023, Mitra et al.[2] published results of their study in which they analyzed data from two SAINT studies: 1) a double-blind randomized clinical trial in which patients with TRD received either active or sham SAINT; and 2) an open-label clinical trial in which patients with TRD received active SAINT. They also analyzed brain-wide signaling patterns in control subjects not experiencing MDD. The researchers found that in the first trial, active SAINT caused “specific directed-signaling shifts in the left DLPFC and bilateral ACC,”[2] but the sham SAINT did not. They found similar effects in the open-label trial. Moreover, Mitra et al. determined that “Whereas the temporal shift of the left DLPFC is not related to treatment efficacy, the temporal shift in the ACC with respect to brain regions including the anterior insula, lateral prefrontal cortex, and temporoparietal junction is correlated with symptomatic improvement.”[2] The evidence indicates that SAINT acts to reverse abnormal signaling patterns in the brain. Mitra et al. also found that “Directional signaling shifts in the ACC, but not the DLPFC, predict improvement in depression symptoms, and moreover, pretreatment ACC signaling predicts both depression severity and the likelihood of SAINT treatment response.”[2] These results indicate that the ACC-based directed signaling patterns in rs-fMRI is a potential biomarker of MDD, and a more potent one than just measuring correlations in activity between brain regions. The researchers concluded that additional research is needed to study whether “directional signaling is altered in subgenual ACC and other brain regions that have been previously implicated in MDD”[2] and “to determine whether modulation of the anterior insula can be utilized for antidepressant effect.”[2]
Batail et al.[3] published results in 2023 from a randomized controlled trial comprising 24 patients (12 active and 12 sham)[1] in which they investigated the brain functional connectivity (FC) changes after using SAINT. The protocol used in the study “resulted in a high remission rate of 57.1% immediately after five days of treatment and 46.2% remission at one-month posttreatment.”[3] After five days of treatment, researchers found changes in three pairs of brain connections: the amygdala-DMN FC (default mode network), the amygdala-SN FC (substantia nigra), and the striatum-SN FC (substantia nigra). Important findings emerged from the study: 1) after SAINT, FC changes supported improved regulation of emotion and reward processing; and 2) amygdala-centered network changes are related to the therapeutic effect of SAINT. Batail et al. also tested the promise of a relationship between FC and clinical outcomes and explored any FC change following active stimulation in comparison to a control group.
The most notable finding from the study was the effect of SAINT on the connection between the amygdala and the DMN. The study results indicate that patients who showed greater increases in amygdala-DMN connectivity and greater decreases in amygdala-SN connectivity experienced better clinical outcomes. Also, the posttreatment brain connectivity patterns in treated patients became more similar to those of healthy control subjects. These changes were noticeable at the one-month follow-up, which suggests the SAINT treatment may have lasting effects. In addition, the research findings support the premise that the amygdala-DMN connectivity dysfunction is an underlying contributor to TRD. This study reported “the first evidence of downstream effects on brain functional connectivity of a rapid acting and highly effective high dose, accelerated iTBS [intermittent theta-burst stimulation] protocol.”[3] Batail et al. suggest further investigation with a larger sample size is warranted to confirm these preliminary results.
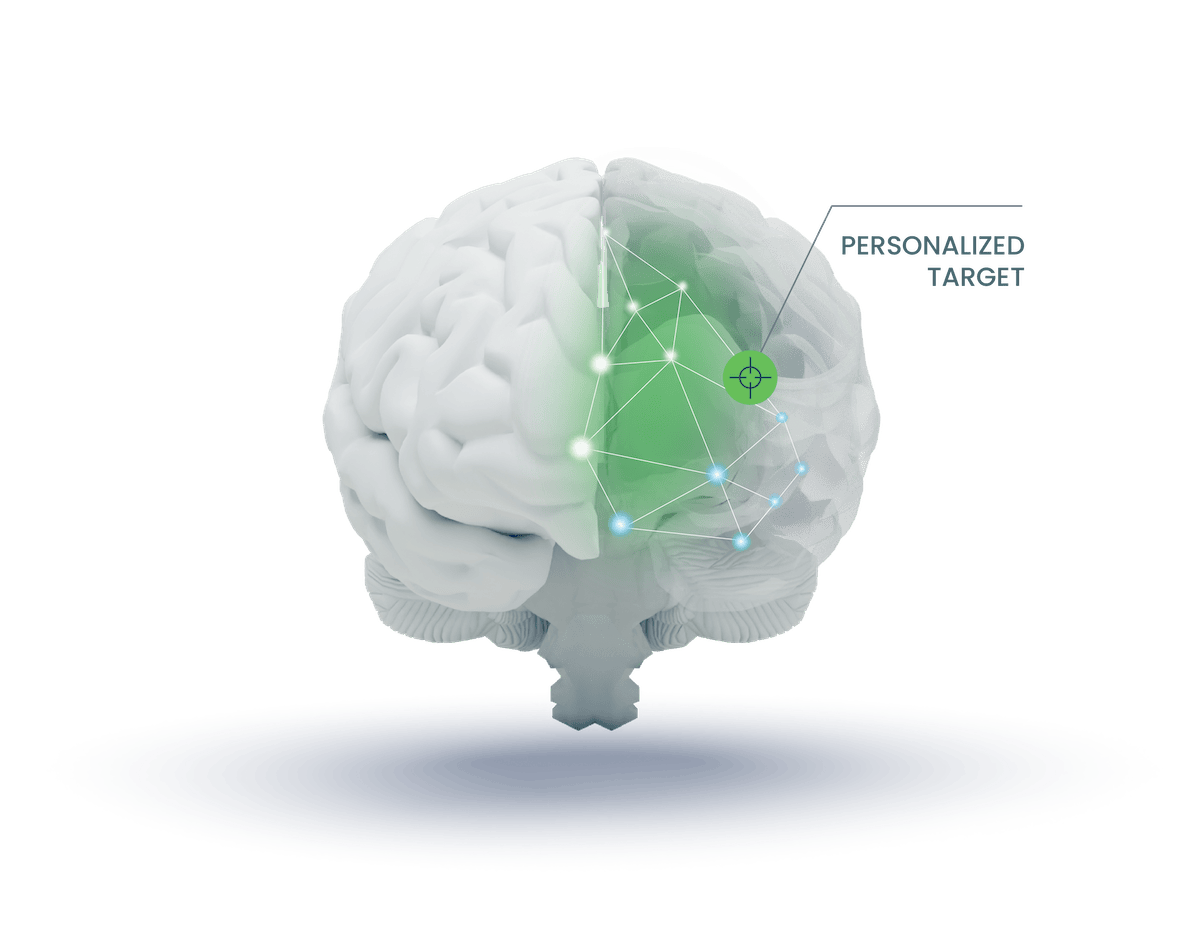
A study by Gajawelli et al.[4] published in 2024, explored how SAINT affects brain activity. Using data from a double-blind trial of 24 participants (12 active, 12 sham), researchers analyzed brain scans taken before SAINT treatment, immediately after, and one month later. The treatment targeted the patient’s left DLPFC. Posttreatment, researchers found increased negative connectivity between the stimulation target and the DMN. These connectivity changes persisted at the one-month follow-up and correlated with improvements in depression symptoms. Targeted stimulation of the L-DLPFC in active participants resulted in significant changes in FC in DMN-associated regions of interest post-treatment. The study results provide “the first evidence of a SAINT-induced biological effect in a sham-controlled trial using a target-based FC approach.”[4]
Targeting of the L-DLPFC in Gajawelli et al.’s study was “predicated on identifying clusters that are maximally negatively connected to the sgACC [subgenual anterior cingulate cortex], for which there remains an abundance of evidence supporting baseline target-sgACC functional connectivity as a strong predictor of antidepressant response.”[4] The significance of Gajawelli et al.’s research is that it may “advance understanding of the biological mechanisms underlying the antidepressant effect of SAINT following a full course of treatment.”[4] Future research should evaluate the downstream prefrontal cortex FC changes after using SAINT to the L-DLPFC target site.
Taken together, these studies provide compelling evidence that SAINT therapy measurably alters brain network dynamics in ways that align with improved emotional regulation and recovery. As our understanding deepens, these findings may help establish imaging-based biomarkers that guide and personalize treatment, ultimately advancing the field of precision psychiatry. Although further research is needed, the neuroimaging data to date clearly underscores SAINT’s potential as a transformative therapy and a window into the biological mechanisms involved in depression.
-
Yale Medicine. Major Depressive Disorder (MDD). ↩︎ ↩︎
-
Mitra A, Raichle ME, Geoly AD, Kratter IH, Williams NR. Targeted neurostimulation reverses a spatiotemporal biomarker of treatment-resistant depression. Proc Natl Acad Sci USA. 2023 May 23;120(21):e2218958120. ↩︎ ↩︎ ↩︎ ↩︎ ↩︎ ↩︎
-
Batail JM, Xiao X, Azeez A, Tischler C, Kratter IH, Bishop JH, et al. Network effects of Stanford Neuromodulation Therapy (SNT) in treatment-resistant major depressive disorder: a randomized, controlled trial. Transl Psychiatry. 2023 Jul 3;13(1):240. ↩︎ ↩︎ ↩︎
-
Gajawelli N, Geoly AD, Batail JM, Xiao X, Maron-Katz A, Cole E, et al. Increased anti-correlation between the left dorsolateral prefrontal cortex and the default mode network following Stanford Neuromodulation Therapy (SNT): analysis of a double-blinded, randomized, sham-controlled trial. Mental Health Res. 2024 Jul 6;3(1):35. ↩︎ ↩︎ ↩︎ ↩︎
