The Depression Treatment Cycle
Madison Lawrence
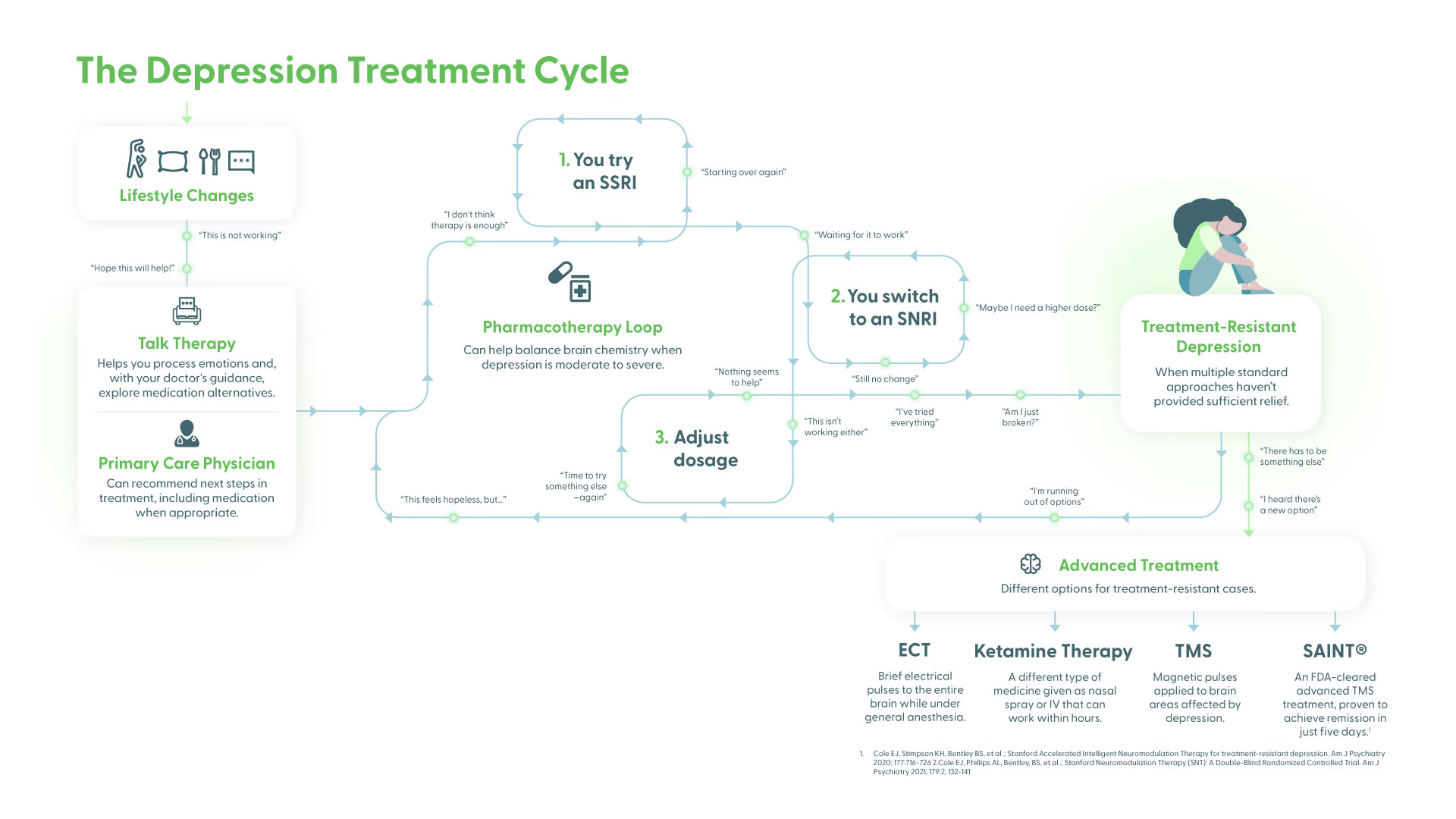
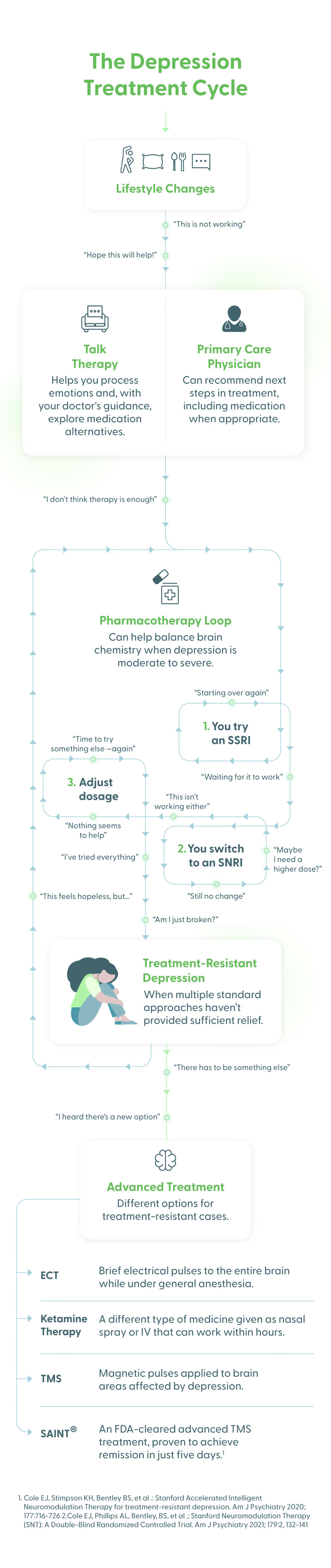
Depression affects each person differently, and there’s no single treatment that works for everyone. Recovery is often a process of trying different approaches, and it can feel like stepping onto an unfamiliar path without knowing exactly where it will lead. To make this journey easier to understand, the team at Magnus Medical created this infographic to map out the many paths people might take on their journey toward better mental health. The road is rarely straight, and often, people with depression will need to explore more than one option to find what works for them. But with persistence, you can find relief from your symptoms.
Awareness: The Beginning of the Journey Toward Wellness
Realizing that you need help and deciding to seek treatment are crucial and courageous first steps on the path toward feeling better. Common symptoms of depression include persistent sadness, loss of motivation, fatigue, changes in sleep or appetite, and difficulty concentrating. Recognizing these signs is the start of your journey to improved mental health.
Paths to Recovery From Depression
Lifestyle Adjustments
Small changes to your daily life can sometimes lift your mood. If these adjustments feel manageable, they may make a meaningful difference, and they often enhance the effectiveness of treatment approaches such as therapy or medication.
- Exercise: Regular movement releases endorphins and improves brain chemistry linked to mood.
- Sleep: Good-quality sleep is crucial for emotional balance. Sticking to a consistent bedtime routine helps restore energy and focus.
- Stress Reduction: Mindfulness practices, journaling, and deep breathing exercises can reduce stress hormones and create mental calm.
Talk Therapy
Therapy is one of the most common starting points for treating depression. Working with a trained professional provides tools to better manage emotions, curb negative thinking, and address underlying issues.
- Cognitive Behavioral Therapy (CBT): Focuses on recognizing harmful thought and behavioral patterns and replacing them with healthier ones
- Interpersonal Therapy (IPT): Concentrates on improving relationships and easing conflicts that may contribute to depression
- Dialectical Behavior Therapy (DBT): Teaches skills to manage overwhelming emotions and strengthen interpersonal bonds
- Mindfulness-Based Cognitive Therapy (MBCT): Combines mindfulness practices with CBT techniques to prevent relapse and stop cycles of negative thinking
- Peer Support: Talking with people who have faced similar struggles through support groups or peer counseling can ease feelings of isolation.
While therapy alone helps many, it’s often combined with medication or other treatment options for more persistent or severe cases.
Medication
When depression is moderate to severe, medication may be recommended. These treatments work by adjusting brain chemistry to ease symptoms, though finding an effective option can take time.
- SSRIs (Selective Serotonin Reuptake Inhibitors): Medications like fluoxetine (Prozac), sertraline (Zoloft), and citalopram (Celexa) increase serotonin levels, often with relatively mild side effects.
- SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors): Drugs like venlafaxine (Effexor) and duloxetine (Cymbalta) boost both serotonin and norepinephrine to improve mood and energy.
- Atypical Antidepressants: Options like bupropion (Wellbutrin) or mirtazapine (Remeron) work through different mechanisms and may suit people who don’t respond well to SSRIs or SNRIs.
- Tricyclics and MAOIs: Older types of antidepressants, such as imipramine or phenelzine, can be effective but often come with more significant side effects or dietary restrictions.
Medication is typically most effective when paired with therapy or lifestyle changes. However, for many people, medication doesn’t work well enough to provide relief for their symptoms; a 2023 analysis found that only 25% of people achieved remission with their first antidepressant, and just 35% had success after trying four different medications. If you’ve gone this route and haven’t had success, you’re far from alone.
Advanced Interventions
Newer medical interventions can offer hope for people who haven’t had success with treatments like therapy and medication. These approaches are usually considered when depression is severe, persistent, or resistant to conventional treatments. These treatments can be highly effective for many and are administered under close medical supervision.
- Transcranial Magnetic Stimulation (TMS): TMS is a noninvasive procedure that uses magnetic pulses to stimulate specific areas of the brain involved in mood regulation. Conventional TMS sessions take place in a clinic over the course of six to nine weeks, and a recent double-blind clinical trial showed a 36% remission rate for this treatment. A more advanced form of TMS, called SAINT® Neuromodulation Therapy, is completed over the course of five days. This accelerated treatment has shown impressive results in a double-blind trial, with 79% of patients treated with SAINT entering full remission from their depression.
- Ketamine Therapy: This drug was originally used as an anesthetic and approved by the FDA in 1970 for use on the battlefields of the Vietnam War, but decades later, clinicians accidentally discovered its antidepressant effects. At low, controlled doses, esketamine, a medication derived from ketamine, can rapidly reduce depressive symptoms, particularly in treatment-resistant cases. Esketamine is administered as an FDA-approved nasal spray (sold under the brand name Spravato) with medical supervision. While common medications for depression block serotonin reabsorption in the brain, causing a gradual buildup of serotonin that can take weeks to cause a noticeable effect, esketamine instead increases levels of glutamate, a neurotransmitter that helps brain cells communicate, producing symptom relief within hours. However, while esketamine acts more quickly, a recent double-blind trial found that only up to 21% of study participants experienced remission, and the drug’s effects don’t appear to last as long.
- Electroconvulsive Therapy (ECT): ECT is a medical procedure in which brief electrical pulses are delivered to the brain under anesthesia to trigger a generalized seizure. A full course of ECT usually involves a series of treatments, typically two to three sessions per week for a total of six to 12 sessions, depending on the patient’s individual needs and response to the treatment. While ECT may cause side effects such as short-term memory changes, modern procedures are carefully monitored and have provided relief for many patients who did not respond to other treatments, with remission rates reaching around 50%.
There’s no single “right” path for treating depression. Some people improve with lifestyle changes and therapy alone, while others may need medication or more advanced treatment options. Many find the best results through a combination of approaches, and for some, newer treatments like accelerated TMS are necessary or preferred.
If you or someone you know is experiencing depression, the most important step is reaching out to a health professional who can guide you toward the right treatment plan. However, if you are having thoughts of suicide or experiencing a crisis right now, please call or text 988 to reach the Suicide & Crisis Lifeline.
Sources:
- https://www.mayoclinic.org/diseases-conditions/depression/diagnosis-treatment/drc-20356013
- https://depressioncenter.org/outreach-education/depression-center-toolkit/not-feeling-well/know-your-treatment-options-0
- https://www.webmd.com/depression/recovery-lifestyle
- https://www.nami.org/about-mental-illness/treatments/ect-tms-and-other-brain-stimulation-therapies/
- https://healthcare.utah.edu/healthfeed/2023/02/fast-facts-about-ketamine-depression

Explore more
Read new insights, patient stories, and updates about personalized neuromodulation treatment for major depressive disorder.